Acute kidney injury (AKI) describes a sudden, temporary decrease in kidney function. Normally, the kidneys’ job is to remove waste and excess water from your blood. AKI is defined as a decrease in as a change in the kidney function. Doctors often diagnose change in kidney function based on a change of a blood test called the creatinine and/or decrease in the amount of urine made. Creatinine is one test that we can use to help us estimate kidney function. Creatinine is checked through a blood test. When your kidneys are not working well as a result of AKI, there is a buildup of waste products in your body and children may develop issues with fluid, blood pressure and electrolyte balance.
What does AKI mean?
How common is AKI?
AKI is very common in children admitted to the NICU. The risk depends on the reason why a baby is taken care of in the NICU. For example, the risk of AKI increases as babies are born very prematurely. For example, the biggest studies of AKI in the NICU found that AKI occurs in 1 in 5 high risk babies born 34 weeks but almost 2 in 5 babies born <28 weeks.
The risk is also higher in several groups of infants, including:
- Infants who are born very prematurely
- Infants that needed a major surgery
- Infants have a critical congenital heart disease
- Infants with a difficult delivery (perinatal or hypoxic injury) who are treated with therapeutic hypothermia (“cooling”)
- Infants with sepsis or infection in their intestine (called NEC or necrotizing enterocolitis)
How do we recognize AKI?
Acute kidney injury (AKI) is usually diagnosed by blood testing (an increased creatinine) or decreased urine output. Creatinine is a waste product that is normally removed by the kidneys, so a higher number often means that the kidneys are not doing their job correctly. Unfortunately, this is not always an accurate measure of kidney function in babies, so we have other ways of diagnosing AKI – we sometimes use other blood or urine tests.
Common symptoms in babies with AKI are low urine output, high blood pressure, and edema (swelling due to fluid buildup). AKI may also be diagnosed from abnormal levels of electrolytes like sodium, potassium, calcium, and phosphate.
In babies that are at risk for AKI, the team will monitor fluid status and for signs or symptoms of kidney injury and will often check lab tests (like the creatinine) to diagnose.
What causes AKI?
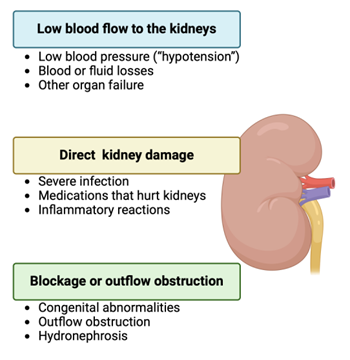 AKI can have many different causes in babies, but we can divide it into three big categories:
AKI can have many different causes in babies, but we can divide it into three big categories:
- Low blood flow to the kidneys:
- Low blood pressure (called “hypotension”)
- Blood or fluid losses
- Other organ failure
- Direct damage to the kidney. Some diseases and conditions can cause damage directly to the kidneys and lead to AKI. Some examples include
- Severe infection
- Blockage of the urinary tract. This is less common but can be due to differences in the way the urinary tract was formed, leading to narrowing (may be pre-natally diagnosed with extra fluid in the kidney, which is called hydronephrosis).
How do we treat AKI?
The way we treat acute kidney injury (AKI) usually depends on what is causing the kidney issues, and as a result there is a wide range of possible treatments. This often includes:
- Careful monitoring of intake (milk/formula/intravenous fluids), output (urine), and weights to ensure a healthy amount of fluid in their body.
- A feeding plan may be put in place to make sure the patient is getting the right balance of all the nutrients they need.
- Keeping a healthy fluid balance may also require intravenous fluids and/or medication to help make more urine (diuretics)
- AKI treatment may also involve avoiding or stopping medications that are harmful to the kidneys, if possible. Sometimes this is not possible if a medication is needed to treat another condition or disease.
- Severe AKI that cannot be treated with these measures may require dialysis. Dialysis can be performed either through a blood vessel (hemodialysis or continuous renal replacement therapy) or through the abdomen (peritoneal dialysis). This allows removal of waste products and fluid while the kidneys recover from their injury. Dialysis does not treat AKI but allows the kidneys time to recover while the dialysis machines do their job.
Why does AKI matter?
In the short-term (during hospitalization), children and babies with AKI have longer time in the hospital and longer time on the ventilator. They are also at an increased risk of having another episode of AKI.
In the long-term, children with an episode of AKI (especially those who are born early) have an increased risk of chronic kidney disease (CKD) and hypertension during childhood and into adulthood. They are also at higher risk of another more severe episode of AKI if they were to get sick.