In July 1969, Neil Armstrong became the first astronaut to walk on the moon. The Apollo 11 mission lasted about four days. Now over 50 years later, astronauts are making much longer trips into space and looking ahead to the potential for even lengthier space flights that could keep astronauts in space for months and years at a time. That possibility brings a new physical challenge for astronauts to deal with: vision loss.
“When they go on long missions in space that are more than six months, almost 70% of astronauts have something called Spaceflight Associated Neuro-ocular Syndrome,” said Tasneem Sharma, PhD, assistant professor of ophthalmology at Indiana University School of Medicine. “On earth, gravity is pulling cerebral spinal fluid down from the brain and behind the eye. But in situations in space where there is no gravity, that doesn’t happen. There is a fluid shift and a change in pressure of that fluid in the brain. As astronauts spend longer and longer in microgravity, then that fluid increases in the brain and can impact their eyes, changing the focus of the eye as a flattening from the back of the eye happens.”
Sharma said when that change happens, astronauts’ vision changes, too, causing them to need reading glasses or other interventions. Thanks to a grant in 2019 from NASA’s Translational Research Institute for Space Health (TRISH) program, Sharma has developed a way to test different pressure changes on the back of the eye to study these effects.
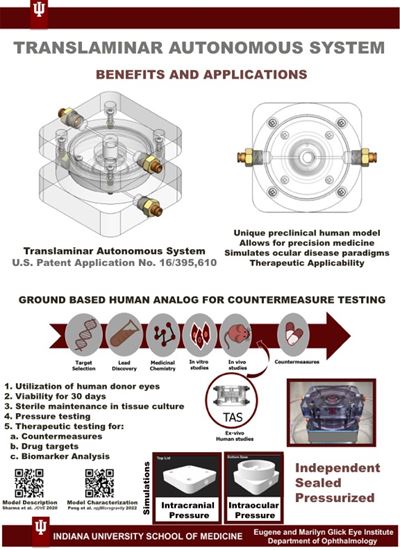
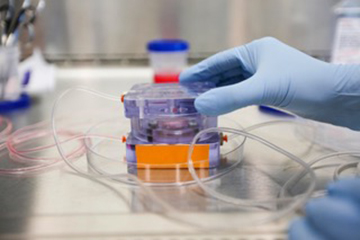
“I have a human eye model and use donor eyes from human patients,” Sharma said. “We put it in a system and mimic that increased pressure at different regions of the eye and see what happens.”
Sharma first studied biomedical engineering at the University of Texas as an undergraduate student. While doing an internship on corneal tissue engineering, she began learning more about eye research and eventually decided to pursue a PhD at the University of North Texas. She focused on glaucoma, a condition where the nerve connecting the eye to the brain becomes damaged, causing blindness.
“The eye is part of the brain and makes up the central nervous system,” Sharma said. “We can do a lot of testing with eyes without needing to inject anything in the brain. It’s a whole area that allows us the availability of tissue to do a lot of other unique experiments.”
After earning her PhD, Sharma completed post-doctoral programs at the University of Iowa and the University of North Texas. Her work there involved studying donor eyes by cutting the eye in half and keeping the front of the eye alive to test glaucoma therapies. Then, Sharma had a new idea to keep the back of the eye for other studies.
 “At that time, no one had really been able to take a human retina and keep it alive for long periods yet, because it’s a high-energy requiring tissue,” Sharma said. “We couldn’t really test any therapeutics or do long-term research on it. We were basically discarding the back of the eye when we wanted to do a front of the eye experiment. So, I drew a bunch of diagrams and had a cousin who was a mechanical engineer at the time help make me a 3D design for a pressurized perfused system to keep that part of the eye alive for longer.”
“At that time, no one had really been able to take a human retina and keep it alive for long periods yet, because it’s a high-energy requiring tissue,” Sharma said. “We couldn’t really test any therapeutics or do long-term research on it. We were basically discarding the back of the eye when we wanted to do a front of the eye experiment. So, I drew a bunch of diagrams and had a cousin who was a mechanical engineer at the time help make me a 3D design for a pressurized perfused system to keep that part of the eye alive for longer.”
Creating the model was more difficult than Sharma expected. The back of the eye experiences different pressure than inside the eye, maintain two pressure chambers was challenging to recreate. After hundreds of attempted models over about a year and a half, Sharma finally found one that worked, called the Translaminar Autonomous System.
“I was like okay this is a model. I have it. Now what do I do with it?” Sharma said. “I put a description of my model on a NASA webpage I found, and about six months later, I got a phone call from TRISH.”
TRISH is part of NASA’s Human Research Program, focused on researching and developing new approaches to reduce risks of long-duration space exploration missions, including NASA’s Journey to Mars. When TRISH discovered Sharma’s human eye model, they asked her if it could be used to study Spaceflight Associated Neuro-ocular Syndrome. Sharma eventually received a grant from TRISH to study the syndrome in 2019. Soon after, she joined faculty at IU School of Medicine, and her team published their study results in Nature in October 2022.
“Here on earth, when I’m sitting, I have a different pressure in my brain than when I’m standing or lying down and sleeping,” Sharma said. “But in space, there’s microgravity, which causes a constant pressure that does not change over time. That is what we tried to mimic with the model, and we found that there are degenerative changes in the eye with that mild, constant intracranial pressure over time. The nerve that connects the eye to the brain also changes shape, and we saw the more we changed the angle of that nerve, the higher the degeneration in the eye.”
In astronauts, Sharma said NASA has found many of them experience some kind of choroidal folds, retinal folds and other clinical findings in the eyes, but for the most part, their symptoms are mild.
 “If they are just in low earth orbit, or on the international space station, these effects do not become significant until astronauts have a mission that is great than six months,” Sharma said. “But then if we’re talking about a long-term mission, more than 6 months, like the Artemis missions on the lunar surface, or the Mars missions, having significant changes in vision can be a mission critical situation.”
“If they are just in low earth orbit, or on the international space station, these effects do not become significant until astronauts have a mission that is great than six months,” Sharma said. “But then if we’re talking about a long-term mission, more than 6 months, like the Artemis missions on the lunar surface, or the Mars missions, having significant changes in vision can be a mission critical situation.”
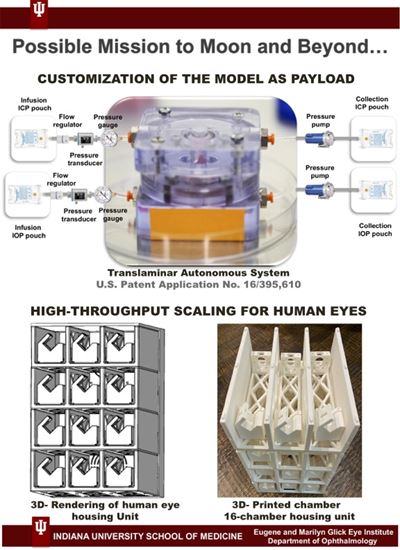
Sharma is currently in the process of applying for a new grant through NASA to continue the research, hoping to next focus on testing other situations that could impact astronauts’ eyes, like how different supplements or antioxidants could help. She could test other environmental conditions like high carbon dioxide and high salt content in the model. In the future, there is even the possibility of doing pre-clinical testing for astronauts in the future, like taking blood or cell samples pre and post flight to generate astronaut stem cells and retinal neurons to test specific therapies or supplements that could work specifically for their biology.
“Using stem cells, we’ve been able to create retinal neurons that we could eventually put in the human eye, then measure the function of the retina and other parts,” Sharma said.
Her team is also collaborating with Loma Linda University for radiation studies and the lunar Zebro team from the Delft University of Technology in Netherlands to send donor eyes to the moon on a lunar rover to study changes in the eye on various parts of the moon.
“There are so many different areas to look at with these experiments,” Sharma said. “NASA wants new and fresh ideas as they focus on long-term space exploration. It’s an exciting field to be part of.”